THE killings of two people could have been predicted or prevented with better mental health care, experts have found.
The risks posed by the mentally unwell killers of Susan Goswell, 66, and Danish tattoo artist Jan Jensen were not properly recognised and dealt with by health professionals, independent panels concluded.
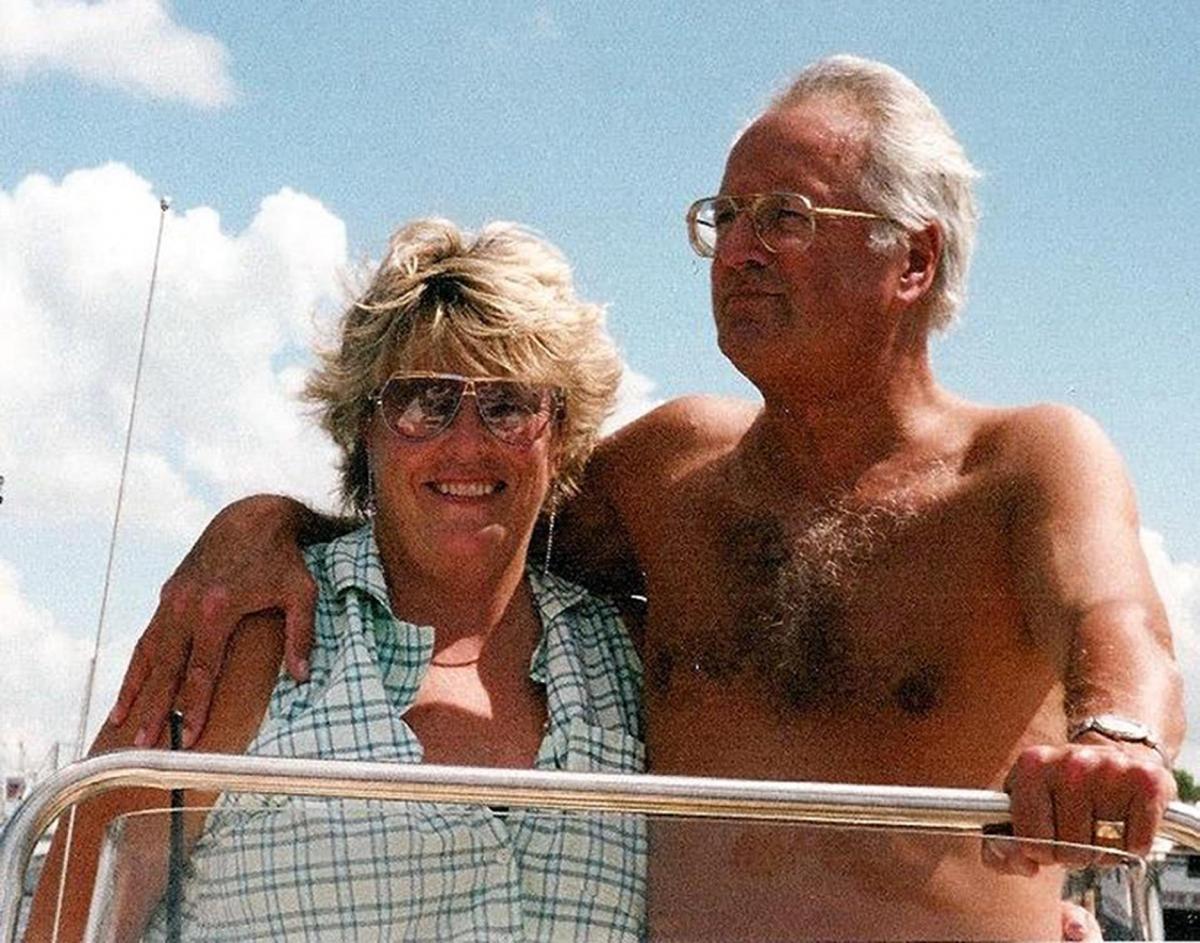
Mrs Goswell was stabbed to death in 2007 by her husband, Roger Goswell, who then killed himself, while Mr Jensen was stabbed to death in 2012 by fellow mental health patient Kayden Smith, 27.
The findings of experts who looked at the cases at the time have emerged in a report reviewing those and the seven other homicides committed since 2007 by patients connected to the Sussex Partnership NHS Trust.
It was commissioned following patient Matthew Daley's killing of grandfather Don Lock, 79, last year, with the trust accepting it had under-diagnosed Daley, 35, and should have listened more to his family.
Mr Goswell, who stabbed his wife to death before killing himself, had managed to persuade healthcare professionals that his threats to kill her were a fantasy and he was a greater threat to himself than to others, the review notes.
Published today, the review, carried out by Caring Solutions consultancy, analyses all the independent reports that were done following each of the nine homicides.
It found several mistakes repeated across the cases, including:
- Criticism of risk assessment in seven out of the nine homicide cases
- Staffs' knowledge of Mental Health Act questioned in "several" cases
- Practice not conforming to local policies and national guidelines in "several" cases
- Problems getting service users to appropriate level of care and treatment.
Colm Donaghy, chief executive of the trust since 2014, said he understood those affected would feel angry and apologised.
He added: "This review sends us a strong message about the need to identify and embed learning when things go wrong in a way that changes clinical practice and behaviour. This goes beyond action plans; it’s about organisational culture, values and leadership."
The trust is improving the way it interacts with patients and their families and changing the way it trains staff on the Mental Health Act, he added.
Asked whether people could have faith in improvements being made given the repetition of mistakes since 2007, he stressed the trust had commissioned the newly published review to learn from it, adding: "The confidence I want to give people is that we will use this report to ensure that we change practice."
The independent review into the case of Matthew Daley has not yet been completed.
- Also read: The Argus leader column - Call for action
MISTAKES MADE GOING BACK YEARS
THE trial of Matthew Daley in May this year opened with a rare admission from the mental health trust involved in his care: We should have listened more to his family, we should have diagnosed him better.
Shortly after Daley was convicted of stabbing to death 79-year-old Don Lock on the roadside as the keen cyclist drove home to his wife, the trust commissioned a review that has now laid bare similar mistakes made in cases going back to 2007. All had been flagged up to the trust at the time or shortly after.
That review, published today, analysed the reports conducted so far into the ten homicides connected to patients at the Sussex NHS Partnership Trust since 2007 – not an unusual rate for an area of its size.
They included the murder of Joe Lewis by Oliver Parsons in Christmas 2014; the killing of Gordon Stalker by Steven Dunne in Elm Grove, Brighton, in 2010; and the killing of Janet Muller after she escaped Mill View psychiatric unit in Hove.
Also included was the killing of Susan Goswell by her husband Roger Goswell in 2007; and of Dutch tattoo artist Jan Jensen by Kayden Smith in 2012.
Incorrectly judging and managing the risk posed by a patient emerges as one of the biggest problems, criticised in seven of the cases and seen as inadequate or “seriously underestimated” in several cases.
Also highlighted was the trust’s own staff not knowing the full extent of their legal powers under the Mental Health Act. And information about criminal records was not always properly understood, the review found.
Reports over the years also repeatedly urged the trust to do more to make sure new procedures were fully implemented, and to do more to involved carers and families in their decisions. The latter made up the third highest number of recommendations in reports dating back to 2007.
The mountain of cases coming into the trust also sometimes meant that some cases were not escalated quickly enough, the review notes, although that has improved.
The reviewers at Caring Solutions UK, commissioned by the trust and NHS England, also flagged up a risky ‘mind-set’ of policies written from the perspective of the service user as a victim rather than perpetrator.
“This tendency occurs in several places,” they said. “Some service users may be perpetrators of violence, exploitation and abuse, and trust policies should reflect that reality.”
They found that of 100 improvements urged over the years, the trust was able to show it had fully embedded one third of what was required, and other parts to a lesser extent.
They added they had seen some changes repeated over time and different services, suggesting they had not been fully implemented in the first place.
Colm Donaghy, chief executive of the trust since 2014, accepted the recurrence of mistakes meant “some of the themes that have come from the recommendations haven’t necessarily been dealt with in the way they should have been, and that’s not acceptable”.
Risk assessments were changing, he added, including by having senior clinical staff get together more often to share opinions and support. Mr Donaghy said training on the Mental Health Act was being changed so it took place in the classroom rather than by computer, and particular focus given to use of the act to try and get patients to take their medication. He and the report also note the trust has committed to the “Triangle of Care” a nationally recognised approach for involving families of mental health patients in their care.
Asked whether he thought he had done enough to improve things during his tenure, Mr Donaghy said: “It’s about actually ensuring that we have a human response to this, that we have a human, cultural, behavioural response as well, which is something I believe I have reinforced very strongly.”
EXPLICIT ABOUT HIS THREATS TO KILL
ROGER Goswell had been released from the Priory psychiatric unit ten days before he killed his wife and then himself.
The 66-year-old property developer had become obsessed with whether his wife Susan Goswell, 63, was a virgin when they married 46 years earlier, a review found, and had tried to kill himself, for the first time, with sleeping tablets and the car exhaust pipe a few weeks earlier.
The family were terrified about his threats to kill his wife and said so to his consultant psychiatrist at the Priory’s Harold Kidd unit.
The couple’s eldest daughter, Sarah Bevan, had emailed professionals begging for her father’s case to be taken seriously.
She had described her father as being a clever and violent man who had expressed a desire to kill his wife and the man she had an earlier relationship with.
She said she was worried about what would happen if her father was discharged, explaining that he had always been violent with all of his children: kicking, punching and whipping their heads against the wall.
The daughter said he suffered from extreme mood swings, could be charming and violent, and that his word could not be trusted.
Yet Mr Goswell, known in his neighbourhood as an intimidating bully with aspirations to be a “country gent”, was able to persuade professionals otherwise.
“Here the perpetrator was quite explicit about his threats to his wife and when questioned was able to persuade healthcare professionals that this was his fantasy and that he was a greater threat to himself than to others”, a new review into the case has found.
“The service user’s adult children provided information about his previous violent behaviour.
“This case probably also represents an instance of healthcare professionals concentrating on the service user rather than seeing him or her as part of a wider set of relationships as would be suggested in a domestic abuse policy.”
Mrs Goswell was found dead at their home in West Chiltington on December 23, 2007. Her husband had stabbed her then had hit her over the head with a mallet.
Her husband then killed himself by smashing his Smart car into a tree near their home.
HEALTH PROFESSIONALS SHOULD HAVE SEEN RISK POSED BY KILLER
KAYDEN Smith, 28, met Jan Jensen, 52, when they were both voluntary patients at Langley Green Hospital in Crawley in August 2012.
Smith invited Mr Jensen back to his flat in Belmont Close, Hassocks, a few days later, where, suffering from severe delusions, he stabbed him to death in a chair. Smith was committed to a secure hospital in July 2013 after admitting manslaughter by diminished responsibility.
An investigation panel found the killing was preventable if professionals had grasped the risk he posed.
A review into the case found: “The service user was not effectively managed by the healthcare team; they were thought not to have assessed the level of risk posed properly and if the service user had been assessed as high risk then a management plan would have been triggered.
“In the panel’s view there was known evidence of risk factors.”
However, experts said the killing itself was not predictable because there was “nothing in his words, actions or behaviour which suggested he was likely to become violent towards the victim”.





Comments: Our rules
We want our comments to be a lively and valuable part of our community - a place where readers can debate and engage with the most important local issues. The ability to comment on our stories is a privilege, not a right, however, and that privilege may be withdrawn if it is abused or misused.
Please report any comments that break our rules.
Read the rules hereLast Updated:
Report this comment Cancel